By: Ruby Fried, University of Alaska Anchorage (UAA), Institute for Circumpolar Health Studies (ICHS); Micah Hahn, UAA, ICHS; Patricia Cochran, Inupiaq Elder, Alaska Native Science Commission; and Laura Eichelberger, Alaska Native Tribal Health Consortium, Research Services, Tribal Water Center
Throughout the COVID-19 pandemic, there has been an urgent need to understand the impacts on daily life in remote Alaska. This NSF RAPID grant, "COVID-19, Knowledge and Health in Remote Alaska Native Communities," is using a community-based and ecosocial approach to identify impacts and responses at individual-, community-, and institutional levels in off-road communities (Krieger 2001). Using an ecosocial approach, our analyses allow for and are interpreted based on the fact that the health and well-being of individuals and populations are dependent on and manifested through multi-level pathways linking biological, ecological, and social organization factors to one another. Study results have, and continue to, provide evidence to tribal health organizations and community leaders to support past and ongoing pandemic responses. This project also contributes to understanding COVID-19 as a biosocial phenomenon (McDade and Harris 2018), recognizing the interaction of health outcomes with various social and structural factors and inequities.
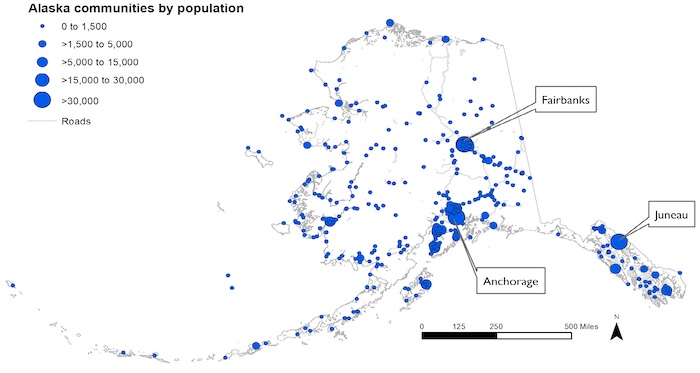
More than 60,000 people live in remote Alaskan communities that are off of the road system and only accessible only by plane, boat, or snowmobile (Figure 1). A multitude of ecosocial factors have increased risk of SARS-Cov2 infection and community spread throughout the pandemic, including inadequate housing and household water insecurity (Eichelberger et al. 2021; Hahn et al. 2022).
We began this study by conducting 23 key informant interviews with remote Alaska community leaders and providers including Alaska Native Elders and tribal and state researchers and providers (September–December 2020). These interviews revealed many immediate and long-term impacts of the pandemic, as well as the positive responses that can be supported during this and other future crises. Major concerns included health and wellbeing, basic needs and services, information needs, economic stability and hardship, and political and power inequalities (Eichelberger et al., in review).
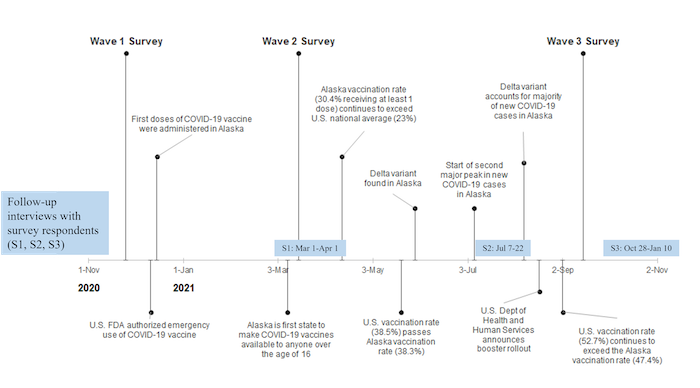
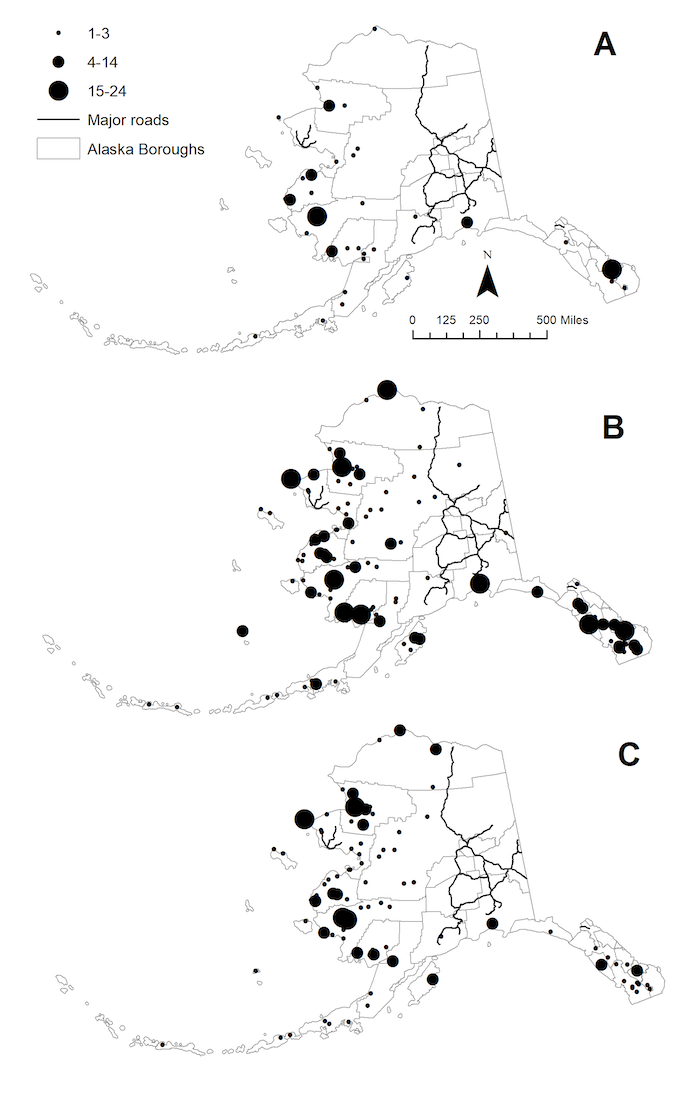
Based on these initial interviews, we designed an online survey that was deployed through three waves, beginning in November 2020, with each followed by in-depth interviews that represented a subset of survey participants (Figure 2). Total survey and in-depth follow-up interviews represented over 1,000 remote Alaskan residents in over 100 communities across all major regions of the state (see Figure 3 below).
Significant Findings
The results of this longitudinal study, described below, provide evidence of how the COVID-19 pandemic is unfolding within a context of syndemic vulnerability, and how the remoteness of these communities has been both a source of vulnerability and protection throughout the pandemic.
The COVID-19 pandemic has affected access to basic needs, including food.
Both key informants and survey respondents who participated in follow-up interviews have described the negative impacts of the pandemic on basic needs, including childcare, healthcare and medicine, water, and food (Eichelberger et al., in review). In particular, Wave 1 and Wave 2 survey and interview data collected between November 2020 and March 2021 revealed that the pandemic negatively impacted store-bought food access through travel and transportation restrictions (ferry and postal service), reduced variety and amount of food in local stores, reduced store access, increased food prices, and panic shopping (Fried et al., in review). However, survey data showed that locally available traditional/subsistence food access was comparatively less affected, with fewer respondents citing difficulty accessing traditional/subsistence foods compared to store-bought foods. Interview data showed that local food sharing likely contributed to this notable difference (Fried et al., in review) These food-related dynamics are an example of both the risk and resilience factors present in remote Alaskan communities.
Trends in vaccine acceptance, hesitancy, and risk perceptions have changed between November 2020 and September 2021.
Prior to vaccine availability, slightly over half of survey respondents showed early potential vaccine acceptance (November/December 2020), with the highest rate among those over the age of 65 years. By March 2021, 80.7% of participants reported receiving the COVID-19 vaccine or planning to get one. Of the unvaccinated, reasons for not getting a vaccine included concerns about side-effects and not trusting the vaccine. By September 2021, 88.5% of survey respondents were fully vaccinated and 79.7% said they would get the booster when eligible. Misconceptions about COVID-19 vaccines included whether they were recommended for pregnant women, and effects on fertility and DNA (Hahn et al. 2022). Follow-up interviews with 37 survey respondents indicated that interpersonal interactions were of particular importance in fostering acceptance among those who were hesitant to get a vaccine (Eichelberger et al. in preparation).
Traditional and cultural activities, as well as organizational and structural initiatives, have helped remote residents cope with pandemic-related disruptions and increased stress. Interviewees throughout the study have described supportive responses at individual, community, and organizational levels that mitigated some of the negative impacts of the pandemic. These included regional coordination of pandemic responses across organizations, the ability for tribes to restrict entry to their communities, and caring for others (particularly Elders). Many identified traditional and cultural activities as particularly important, including the translation of prevention messages into local languages and creative activities. Indeed, although the pandemic affected in-person practices of sharing, individual access to traditional foods was less affected and may have increased in importance due to store-bought food shortages.
COVID-19 is still here—what are we doing now?
As of January 2022, we are currently finalizing analyses on the third round of survey follow-up interviews, as well as longitudinal analyses to examine stress and coping, and vaccine acceptance/hesitancy, currently and throughout the pandemic. In addition, through community conversations as part of this project, our team recently began a new research initiative in northwest Alaska to understand the decision-making processes and motivating factors of individuals in vaccine-hesitant populations and those who were once "hesitant" to ultimately accept a COVID-19 vaccine. That initiative is funded in part by the NSF award, RAPID: An Indigenous-Centered Approach to COVID-19 Vaccine Hesitancy and Acceptance.
Overall, this statewide, longitudinal study on remote communities provides a perspective based on the lived experience of Indigenous and non-Indigenous people living in remote Arctic communities, and an opportunity for evidence- and strengths-based responses to the many impacts of COVID-19. The lessons learned may be applicable to other remote Arctic communities, and potentially to any future disruptions caused by public health crises, natural disasters, and other wide-reaching disruptions to daily life.
References
Eichelberger, L. P., S. Dev, T. Howe, D. Barnes, E. Bortz, B. Briggs, P. Cochran, A. Dotson, D. Drown, M. B. Hahn, K. Mattos, and S. Aggarwal. 2021. Implications of Inadequate Water and Sanitation Infrastructure for Community Spread of COVID-19 in Remote Alaskan Communities. Science of the Total Environment.
Eichelberger, L. P., R. L. Fried, P. Cochran, T. Howe, and M. B. Hahn. In review. Understanding COVID-19 as a Lived Experience of Both Syndemic Vulnerability and Community Strengths: Community Leader and Provider Descriptions of the 2020 Pandemic in Remote Alaska.
Eichelberger, L. P., R. L. Fried, P. Cochran, L. Gillott, T. Howe, and M. B. Hahn. In review. "Every person here is needed, we all have our role": Basic Needs and Community Support during the COVID-19 Pandemic in Remote Alaskan Communities.
Eichelberger, L. P., R. L. Fried, P. Cochran, Z. Merritt, and M. B. Hahn. In preparation. "In the beginning, I said I wouldn't get it": Understanding Vaccine Hesitancy and Acceptance in Remote Alaska between November 2020 and July 2021.
Fried, R. L., M. B. Hahn, P. Cochran, and L. P. Eichelberger. In Review "Remoteness was a blessing, but also a potential downfall": Traditional/Subsistence and Store-Bought Food Access in Remote Alaska During the COVID-19 Pandemic. Public Health Nutrition. Submitted 1 November 2021.
Hahn, M. B. Climate Change and Health in Alaska: How do Things Compare with the Lower-48? In Global Change and Human Health: From Science to Practice, 2nd edition; eds. Jay Lemery, Kim Knowlton, and Cecilia Sorenson. Jossey-Bass: San Francisco, CA, 2021.
Hahn, M. B., R. L. Fried, P. Cochran, and L. P. Eichelberger. 2022. Evolving Perceptions of COVID-19 Vaccines Among Remote Alaskan Communities. International Journal of Circumpolar Health.
Krieger, N. 2001.Theories for Social Epidemiology in the 21st Century: An Ecosocial Perspective. International Journal of Epidemiology, 30(4), 668-677. doi:10.1093/ije/30.4.668.
McDade, T. W. and K.M. Harris. 2018. The Biosocial Approach to Human Development, Behavior, and Health Across the Life Course. RSF. 4(4):2-26. doi:10.7758/RSF.2018.4.4.01.
About the Authors
 Ruby Fried, PhD, University of Alaska Anchorage, Institute for Circumpolar Health Studies (ICHS). (rlfried [at] alaska.edu)
Ruby Fried, PhD, University of Alaska Anchorage, Institute for Circumpolar Health Studies (ICHS). (rlfried [at] alaska.edu)
Ruby Fried is an Assistant Professor of Health Science at ICHS. Her work focuses on identifying the drivers of health outcomes in terms of both risk and resilience. Fried's research includes examining the health impacts of traditional foods among Alaska Native people, traditional food security, and other mixed methods projects related to food environments and health disparities with a commitment to active and meaningful community-driven research.
 Micah Hahn, MPH, PhD, University of Alaska Anchorage, Institute for Circumpolar Health Studies (ICHS). (mbhahn [at] alaska.edu)
Micah Hahn, MPH, PhD, University of Alaska Anchorage, Institute for Circumpolar Health Studies (ICHS). (mbhahn [at] alaska.edu)
Micah Hahn is an Assistant Professor of Environmental Health at ICHS. Her research focuses on the health impacts of climate change and climate adaptation and resilience planning in Alaska. She is trained as an epidemiologist and incorporates epidemiological study designs, spatiotemporal exposure assessment, GIS analysis, weather and climate data, ecological predictive modeling, and mixed-methods to answer interdisciplinary, applied questions around climate-related exposures and human-animal-environment interactions.
 Patricia Cochran, Inupiaq Elder, Alaska Native Science Commission. (pcochran [at] aknsc.org)
Patricia Cochran, Inupiaq Elder, Alaska Native Science Commission. (pcochran [at] aknsc.org)
Patricia Cochran, Inupiaq Elder, was born and raised in Nome, Alaska. Ms. Cochran serves as Executive Director of the Alaska Native Science Commission, an organization that brings together research and science in partnership with Alaska Native communities. Ms. Cochran also served as Chair of the 2009 Indigenous Peoples' Global Summit on Climate Change and Co-Chair of the Indigenous Peoples' Global Network on Climate Change. She is the past Chair of the Inuit Circumpolar Council, an international organization representing 160,000 Inuit of Alaska, Canada, Russia, and Greenland; former Chair of the Indigenous Peoples' Secretariat to the eight nation, Arctic Council; and former Arctic Representative to the United Nations Permanent Forum on Indigenous Issues.
 Laura Eichelberger, MPH, MA, PhD, Alaska Native Tribal Health Consortium, Research Services, Tribal Water Center. (lpeichelberger [at] anthc.org)
Laura Eichelberger, MPH, MA, PhD, Alaska Native Tribal Health Consortium, Research Services, Tribal Water Center. (lpeichelberger [at] anthc.org)
Laura Eichelberger is an Epidemiology and Health Research Consultant at the Alaska Native Tribal Health Consortium. Her research integrates methods from anthropology and epidemiology to examine the health effects and lived experiences of household water security, emerging infectious diseases, and climate change. She currently leads projects focusing on the impacts of the COVID-19 pandemic on remote Alaskan communities, assessing the effects of decentralized water and sanitation systems on health and household water security, and identifying community priorities around water quality and safe water infrastructure.
